Community Acquired Pneumonia (CAP)
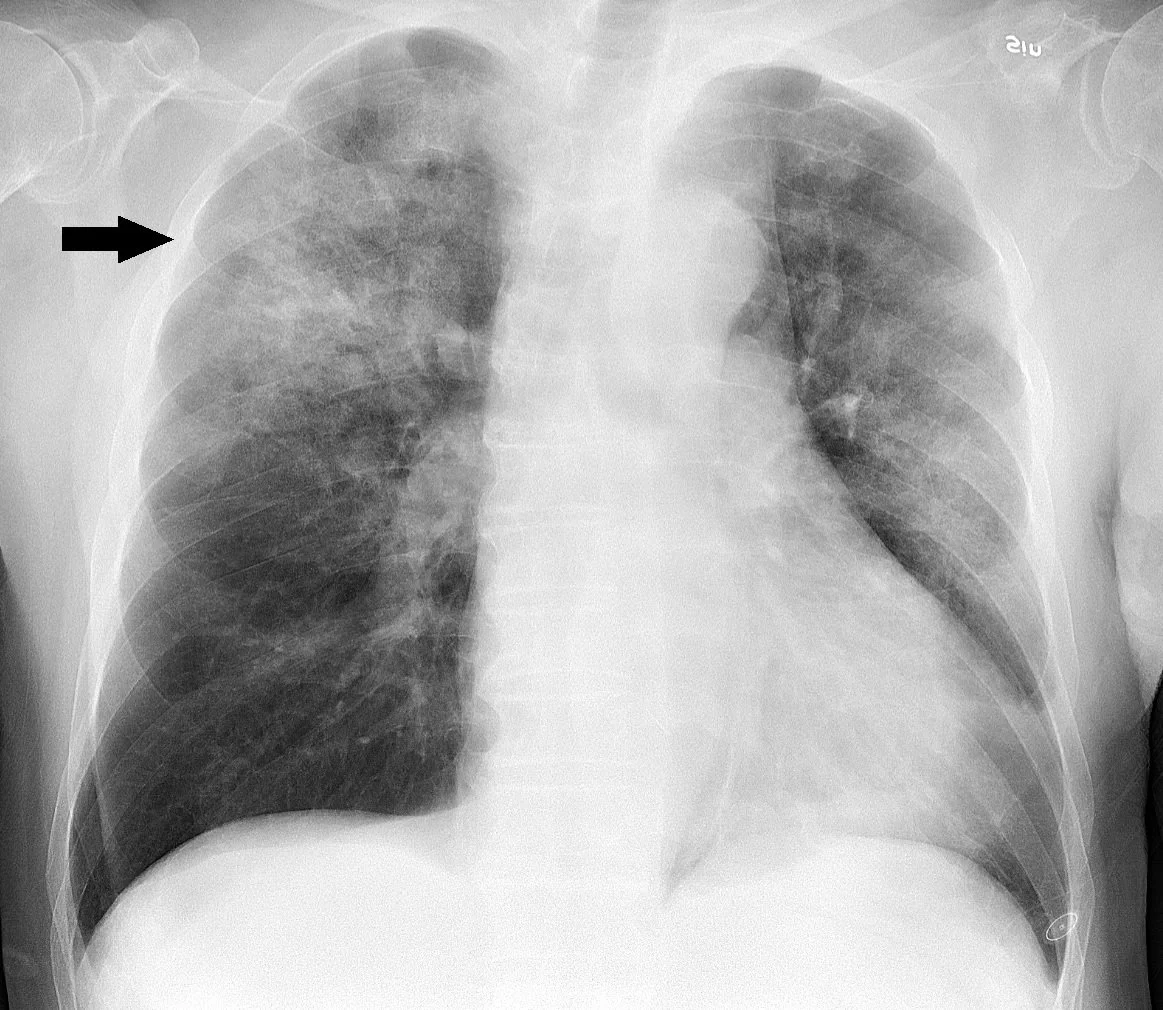
Community acquired pneumonia (commonly abbreviated to “CAP”) is a life-threatening lung infection and CAP is a leading cause of hospitalization and mortality globally.(1,2) It is defined by the presence of respiratory signs and symptoms (cough, sputum production, dyspnea, chest pain), systematic effects (fever, fatigue, diaphoresis, headache, nausea, myalgias), and a new radiographic (chest x-ray) pulmonary infiltrate (See figure 1). A universal diagnostic definition of CAP does not exist.(3)
Despite extensive evaluation, a bacteria or virus is only identified in ~30% of patients.(4) One or more virus are isolated in ~23% of cases, but only 6% are attributable to influenza, the sole CAP virus with an available antiviral treatment (e.g., oseltamivir).(5) The main treatment for CAP is empiric antibiotics and supportive care, including oxygen.(6) Corticosteroids may reduce the inflammatory response to CAP, but clinical trials have demonstrated inconsistent and modest effects, and other therapies are not currently recommended.(7-9) New effective strategies are needed.
Complications from CAP
The incidence of hospitalization for CAP ranges, by country, from 18-290 per 10,000 person-years.(1) In Canada, CAP was the 3rd most common reason for hospitalization in 2019 (69,403 hospitalizations), with an incidence higher than most other high-income countries (214-280 cases per 10,000 person-years).(10,11) In the United States (US), CAP is the 2nd most common cause of hospitalization, accounting for 1.1-1.5 million admissions and up to $40 billion USD annually. CAP incidence increases with age, affecting 2% of US citizens aged ≥ 65 each year. The incidence of CAP is also increased in patients with obesity, chronic smoking, diabetes, stroke, chronic cardiac conditions, and chronic lung conditions.(12,13)
Poor hospital outcomes in CAP are driven by inflammation and thrombotic (blood clotting) responses to infection, leading to thrombosis (deep vein thrombosis or pulmonary embolus) and organ dysfunction.(14,15) Antibiotics and supportive therapy improves outcomes in CAP; however, effective therapies that target the bodies response to the infection are lacking.
Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC)
In the ATTACC trial, which looked at CAP caused by SARS-CoV-2 (COVID-19), we demonstrated that therapeutic-dose heparin, an antithrombotic with anti-inflammatory and possible antimicrobial effects, reduced the outcome of those requiring intensive care unit (ICU)-level organ support (for organ failure) and mortality in non-critically ill patients.16 These findings have been incorporated into Canadian and international clinical practice guideline recommendations. Although both pneumonia caused by SARS-CoV-2 and CAP caused by other infectious agents follow a similar course of illness of inflammation and thrombosis, the potential benefit of therapeutic-dose heparin in CAP is unknown. For more on the ATTACC trial, click here.
References
Ferreira-Coimbra J, Sarda C, Rello J. Burden of Community-Acquired Pneumonia and Unmet Clinical Needs. Adv Ther 2020;37:1302-18.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88.
Flateau C, Le Bel J, Tubiana S, et al. High heterogeneity in community-acquired pneumonia inclusion criteria: does this impact on the validity of the results of randomized controlled trials? BMC Infect Dis 2018;18:607.
Jain S, Self WH, Wunderink RG, et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N Engl J Med 2015;373:415-27.
Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America: 2018 Update on Diagnosis, Treatment, Chemoprophylaxis, and Institutional Outbreak Management of Seasonal Influenzaa. Clin Infect Dis 2019;68:895-902
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med 2019;200:e45-e67.
Siemieniuk RA, Meade MO, Alonso-Coello P, et al. Corticosteroid Therapy for Patients Hospitalized With Community-Acquired Pneumonia: A Systematic Review and Meta-analysis. Ann Intern Med 2015;163:519-28.
Briel M, Spoorenberg SMC, Snijders D, et al. Corticosteroids in Patients Hospitalized With Community-Acquired Pneumonia: Systematic Review and Individual Patient Data Metaanalysis. Clin Infect Dis 2018;66:346-54.
Siempos, II, Vardakas KZ, Kopterides P, Falagas ME. Adjunctive therapies for community-acquired pneumonia: a systematic review. J Antimicrob Chemother 2008;62:661-8.
Inpatient hospitalization, Surgery, Newborn Statistics, 2019-2020. 2021. (Accessed Feb 28, 2022, at https://www.cihi.ca/en/search?query=pneumonia&Search+Submit.)
Nasreen S, Wang J, Kwong J, et al. 1211. Incidence of All-Cause Community-Acquired Pneumonia in Ontario and British Columbia, Canada, 2002-2018; a Canadian Immunization Research Network (CIRN) study. Open Forum Infectious Diseases 2021;8:S695-S6.
Ramirez JA, Wiemken TL, Peyrani P, et al. Adults Hospitalized With Pneumonia in the United States: Incidence, Epidemiology, and Mortality. Clin Infect Dis 2017;65:1806-12.
Pfuntner A, Wier LM, Stocks C. Most Frequent Conditions in U.S. Hospitals, 2011: Statistical Brief #162. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006.
Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol 2013;13:34-45.
Cangemi R, Calvieri C, Falcone M, et al. Comparison of Thrombotic Events and Mortality in Patients with Community-Acquired Pneumonia and COVID-19: A Multicenter Observational Study. Thromb Haemost 2022;122:257-66.